Effect of atrial fibrillation on outcomes in patients with anterior circulation occlusion stroke receiving endovascular therapy
- 1Department of Neurology and Advanced National Stroke Center, Foshan Sanshui District People’s Hospital, Foshan, China
- 2Department of Medicine, Federal University of Santa Maria, Santa Maria, Brazil
- 3Department of Neurology, Radiology, Boston University Chobanian and Avedisian School of Medicine, Boston, MA, United States
- 4School of Medicine, Dentistry and Biomedical Sciences, Queen’s University Belfast, Belfast, United Kingdom
- 5Department of 120 Emergency Command Center, Foshan Sanshui District People’s Hospital, Foshan, Guangdong, China
- 6UCLA Stroke Center and Department of Neurology, University of California, Los Angeles, Los Angeles, CA, United States
- 7Department of Internal Medicine-Cardiovascular, Foshan Sanshui District People’s Hospital, Foshan, Guangdong, China
- 8Department of Neurosurgery, First People’s Hospital of Foshan, Foshan, Guangdong, China
- 9Department of Neurology, Guangdong Provincial Hospital of Integrated Traditional Chinese and Western Medicine (Nanhai District Hospital of Traditional Chinese Medicine of Foshan City), Foshan, Guangdong, China
- 10Department of Research and Education, Foshan Sanshui District People’s Hospital, Foshan, China
- 11Department of Neurosurgery and Advanced National Stroke Center, Foshan Sanshui District People’s Hospital, Foshan, Guangdong, China
- 12Department of Neurology, Guangzhou Eighth People’s Hospital, Guangzhou Medical University, Guangzhou, Guangdong, China
- 13Department of Neurology, The First Affiliated Hospital of Jinan University, Guangzhou, China
- 14Neuro International Collaboration (NIC), Foshan, China
Objective: Atrial fibrillation is one of the major risk factors of ischemic stroke. Endovascular thrombectomy (EVT) has become the standard treatment for acute ischemic stroke with large vessel occlusion. However, data regarding the impact of AF on the outcome of patients with acute ischemic stroke treated with mechanical thrombectomy are controversial. The aim of our study was to determine whether atrial fibrillation modifies the functional outcome of patients with anterior circulation acute ischemic stroke receiving EVT.
Methods: We reviewed 273 eligible patients receiving EVT from January 2019 to January 2022 from 3 comprehensive Chinese stroke centers, of whom 221 patients were recruited. Demographics, clinical, radiological and treatment characteristics, safety outcomes, and functional outcomes were collected. Modified Rankin scale (mRS) score ≤ 2 at 90 days was defined as a good functional outcome.
Results: In our cohort, 79 patients (35.74%) were eventually found to have AF. Patients with AF were elder (70.08 ± 11.72 vs. 61.82 ± 13.48 years, p = 0.000) and less likely to be males (54.43 vs. 73.94%, p = 0.03). The significant reperfusion rate (modified thrombolysis in cerebral infarction 2b-3) was 73.42 and 83.80% in patients with and without AF, respectively (p = 0.064). The good functional outcome (90-day modified Rankin scale: 0 to 2) rate was 39.24 and 44.37% in patients with and without AF, respectively (p = 0.460) after adjusting multiple confounding factors. There was no difference in the presence of symptomatic intracerebral hemorrhage between the two groups (10.13 vs. 12.68%, p = 0.573).
Conclusion: Despite their older age, AF patients achieved similar outcomes as non-AF patients with anterior circulation occlusion treated with endovascular therapy.
1. Introduction
Atrial fibrillation (AF) is the most common non-structural cardiac condition related to ischemic cerebrovascular diseases (Junejo et al., 2020). One of the important risk factors associated with developing structural and non-structural cardiac abnormalities is aging (Yousufuddin and Young, 2019). With the worldwide population aging, the proportion of patients with AF is expected to rise in the coming decades (Kornej et al., 2020). A higher prevalence of AF in middle socio-demographic index countries and the in-hospital embolic recurrence in presumed cardioembolic stroke patients with AF cause a significant rise in medical cost (Arboix et al., 1998). Therefore, studies about the impact of AF on outcomes of thromboembolic stroke are of economic interest.
Atrial fibrillation is associated with poor functional outcomes and increased hemorrhagic complications after intravenous thrombolysis (IVT) (Kimura et al., 2009; Sanak et al., 2010). Bridging IVT improved functional outcomes in non-AF patients, but the benefits did not extend to AF patients (Akbik et al., 2022; Loo et al., 2023). However, the impact of AF on the treatment effect of mechanical thrombectomy (MT) remains controversial. Patients with AF responded significantly better to MT than those without AF did (Lin et al., 2020), while other studies showed that AF experienced worse 90-day outcomes, even in the setting of similar rates of successful reperfusion and independent negative predictors of good long-term functional outcome (Zdraljevic et al., 2022; Kobeissi et al., 2023). In addition, age > / = 80 years was a significant predictor of unfavorable outcomes after EVT for AIS patients with AF (Jiao et al., 2022).
We performed a retrospective study based on a multicenter stroke registry to compare the technical and functional outcomes in acute ischemic stroke patients with and without AF after receiving EVT. We also evaluated the impact of age in AF patients with anterior circulation occlusion after EVT.
2. Patients and methods
2.1. Study population
A hospital-based cohort of 273 subjects who underwent EVT was recruited from three comprehensive stroke centers in Foshan, China from January 2019 to January 2022. The study was approved by the Ethical Board of the Foshan Sanshui District People’s Hospital in China. Medical records were assessed for data on socio-demographic characteristics, clinical features, neuroimaging, and EVT results.
The inclusion criteria for this study were: (1) age ≥18, (2) independent daily living [modified Rankin scale (mRS < 3)] before the index stroke, (3) undergoing EVT within 24 h of symptom onset, (4) presence of intracranial internal carotid artery (ICA) and/or anterior circulations occlusions M1 (MCA-M1) and M2 (MCA-M2) segments of the middle cerebral artery (MCA), or tandem occlusion. Exclusion criteria were: (1) lost to follow-up, (2) other vessel occlusions. Screening and treating AF are two important aspects of managing AF. 12-lead electrocardiogram (ECG) was used for all patients in our hospital, and 24-h ECG (Holter) monitoring was used for all cardiac embolic stroke subgroups. However, post-stroke in-hospital rhythm monitoring was limited by a finite window of observation, which was particularly problematic in the context of intermittent AF. For all AF patients, anticoagulants were used when CT exclude hemorrhage after EVT according to the consensus rule of “1-3-6-12” days. Oral anticoagulants included warfarin and target-specific anticoagulants, also known as direct oral anticoagulants. We usually use the TOAST (Trial of Org 10172 in Acute Stroke Treatment), which includes large-artery atherosclerosis (LAA), cardioembolism (CE), small-artery occlusion lacunar (SAA), stroke of other determined etiology (SOE), and stroke of undetermined etiology (SUE). However, subjected to the condition in the primary hospital, the non-invasive examination was particularly problematic in the screening of patients with intermittent AF, thereby compromising the accuracy of CE, SOE, and SUE.
2.2. Data collection and measurements
Patients’ demographic data (age, sex), comorbidities (AF, hypertension, diabetes mellitus, coronary artery diseases, hyperlipidemia, chronic kidney disease, smoking history, past history of stroke), laboratory tests (triglyceride, low-density lipoprotein, high-density lipoprotein, total cholesterol, and glucose at admission) were recorded. Stroke severity [National Institute of Health Stroke Scale/Score (NIHSS) score at admission], time intervals (door-to-puncture, door-to-recanalization time, last-known-well-to-puncture time, door-to-puncture time, puncture to recanalization time), functional outcomes (NIHSS score after EVT and mRS), and symptomatic intracranial hemorrhage (sICH) were assessed. A favorable functional outcome was defined as mRS 0 to 2 at 90-day follow-up (Yang et al., 2022).
2.3. EVT procedures
The decision to perform EVT was made by the team of vascular neurologists and treating neuroradiologists. Board-certified interventional neuroradiologists performed the EVT procedure. In eligible patients, EVT was performed according to the European Stroke Organization guideline by the European Society for Minimally Invasive Neurological Therapy guidelines (Turc et al., 2019). Mechanical thrombectomy was performed from femoral puncture using a guiding sheath and an intermediate catheter and stent retriever. Substantial reperfusion was defined as modified Thrombolysis in Cerebral Infarction scale (mTICI) 2b or 3 at the completion of the procedure (Chen et al., 2022). Patients were admitted to the stroke unit for close monitoring and observation for at least 24 h postoperatively.
2.4. Statistical analysis
Double data entry and standardized procedures were performed for quality checking. No imputations were made for missing data. The data were then transported to the IBM SPSS software version 26 (IBM Corp., Armonk, NY) for statistical analysis. The Kolmogorov-Smirnov test was used for assessing normality. Categorical variables were represented as proportions, and continuous variables were described as means and standard deviations. A p-value < 0.05 was considered significant in all analyses. As appropriate, we used an independent Student’s t-test and Mann–Whitney U test to compare basic characteristics between groups. The categorical variables were analyzed using Chi-squared (χ2) or Fisher’s exact tests if the expected number was ≤5. We created unadjusted and adjusted binary logistic regression models to determine associations between EVT and the study outcomes adjusted for age and other variables recorded.
3. Results
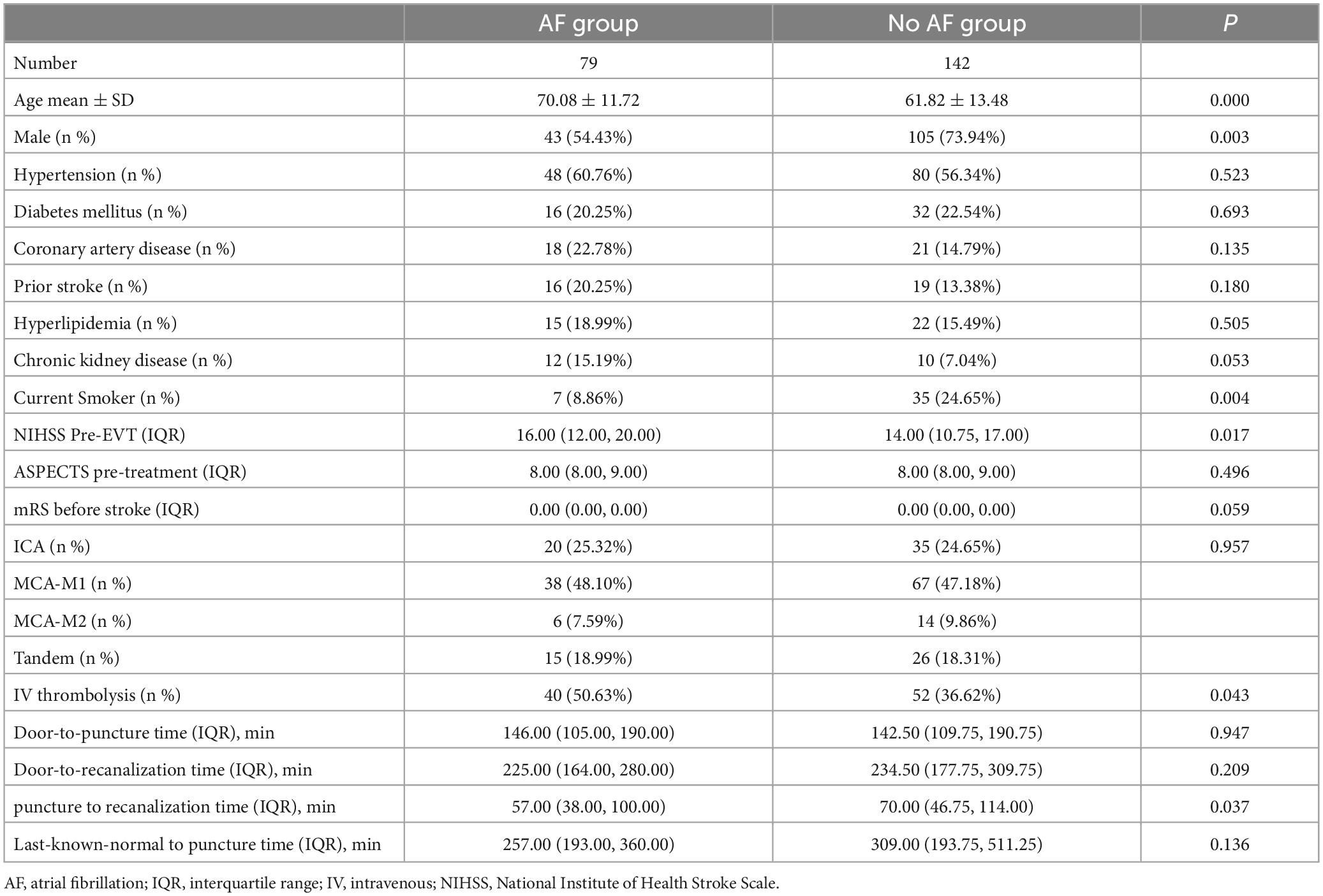
A total of 273 subjects were eligible for the study. Three patients were lost to follow-up due to non-compliance; one patient was excluded because of presentation with occlusion of the M3 segment of the MCA; 40 subjects were excluded due to basilar artery occlusion; eight subjects had other multiple vessel occlusions. 221 patients (79 with AF, 142 without AF) were included in the final study. Table 1 summarizes the characteristics of the study participants.
Comparing the AF group and no AF group, the AF group was older (70.08 ± 11.72 vs. 61.82 ± 13.48 years old, p < 0.001), had fewer male sex [54.43 vs. 73.94% (p = 0.003)], had fewer smokers (8.86 vs. 24.65%, p = 0.004), had higher median NIHSS Pre-EVT (16 vs. 14, p = 0.017), underwent more IV thrombolysis before EVT [50.63 vs. 36.62% (p = 0.043)], but had a shorter median puncture to recanalization time (57 vs. 70 min, p = 0.037). The other baseline characteristics between patients with and without AF did not differ significantly.
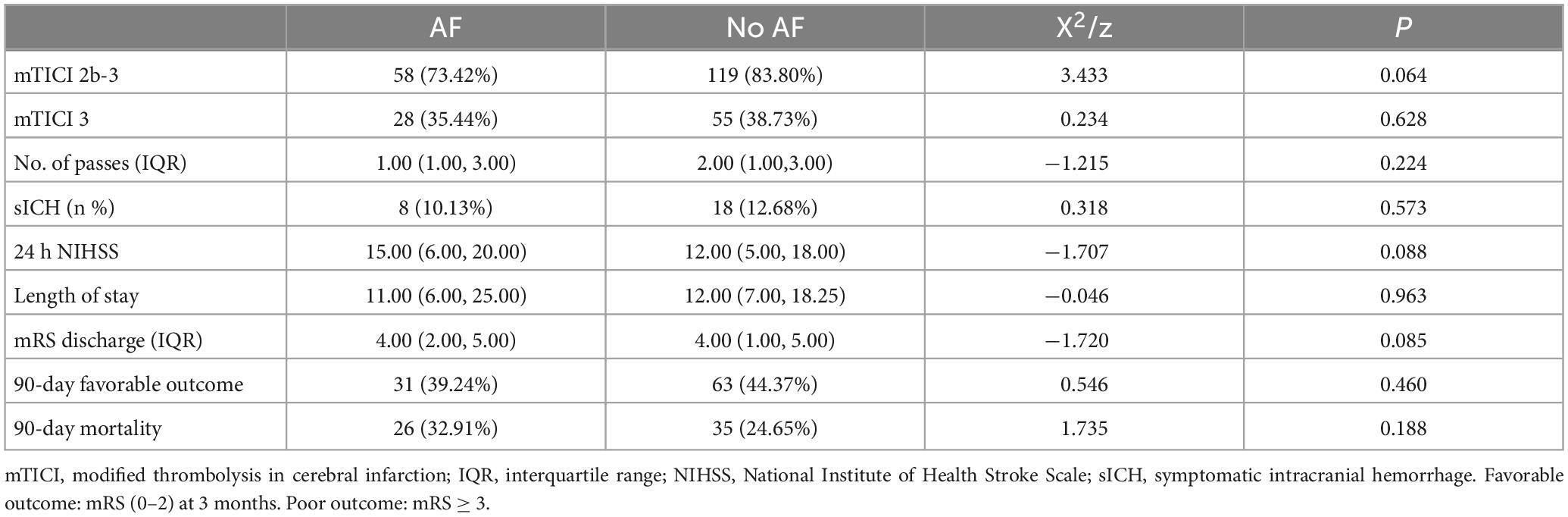
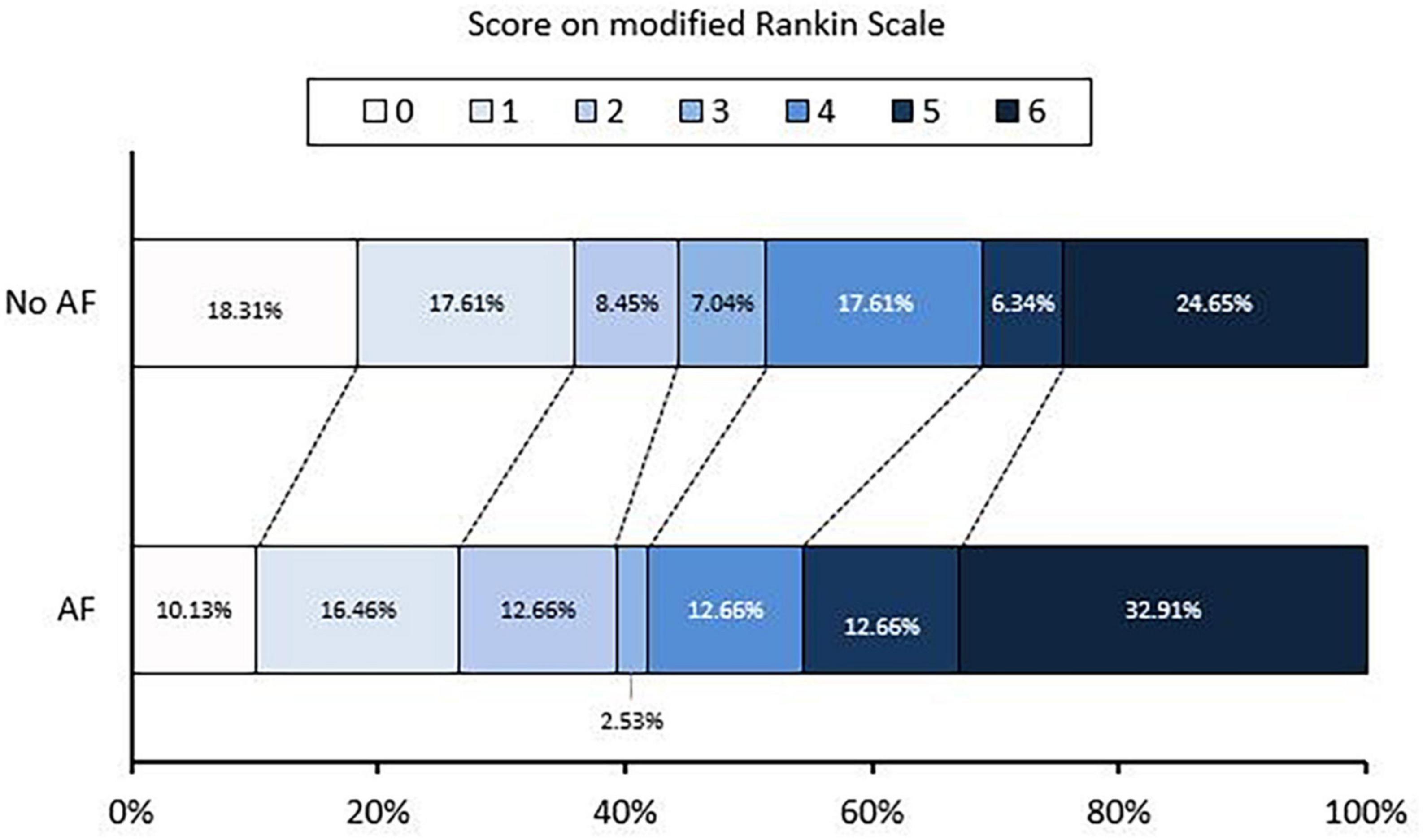
In unadjusted analyses, individuals undergoing EVT with AF compared to those without AF did not present any difference in favorable functional outcomes (90-day outcome 39.24 vs. 44.37%, p < 0.460) (Table 2). Figure 1 depicts the distribution of 90-day mRS in both groups.
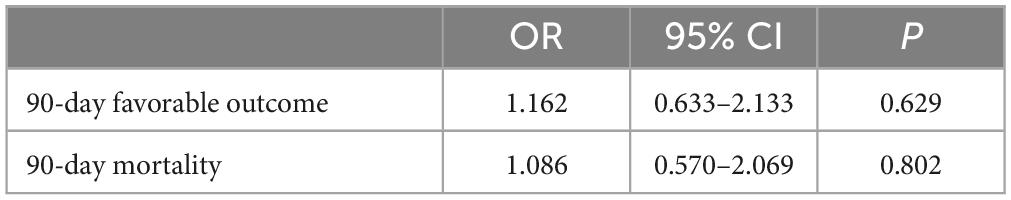
In the binary logistic regression model, we found persistence of the findings of the comparison between the 90-day outcome of AF and non-AF individuals after controlling for other factors. Table 3 provides results of 90-day outcome (p = 0.629) and 90-day mortality (p = 0.802) after adjusting for age (<65 years), which were not significant.
In Table 4, age, male sex, CKD, current smoking history, and mRS before stroke were controlled. Similar to previous findings, there were no statistically significant differences for 90-day outcome (p = 0.482) and 90-day mortality (p = 0.928).
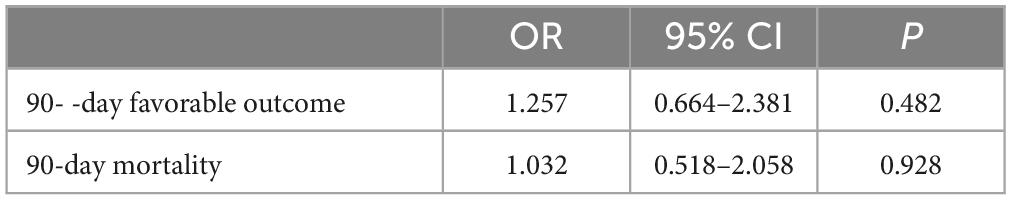
Table 4. Comparison of 90-day outcome (AF group vs. non-AF group) after adjusting age, male sex, chronic kidney disease, current smoking history, and mRS before stroke.
In the last model (Table 5), the variables controlled were age, male sex, chronic kidney disease, current smoking status, NIHSS Pre-EVT, mRS pre-treatment, intravenous thrombolysis, last-known-well-to-puncture time, and puncture to recanalization time. After such controls, no statistically significant differences were found for 90-day outcome (p = 0.461) and 90-day mortality (p = 0.661).
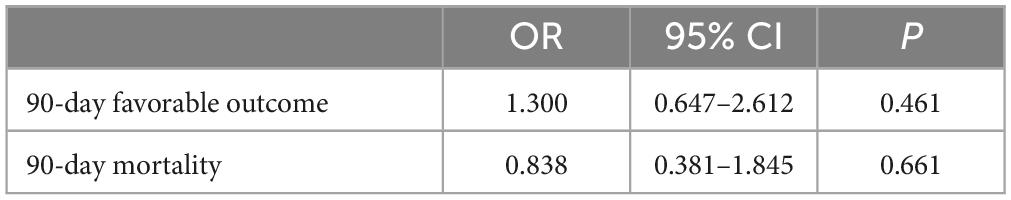
Table 5. Comparison of 90-day outcome (AF group vs. non-AF group) after adjusting age, male sex, chronic kidney disease, current smoking history, NIHSS Pre-EVT, mRS pre-treatment, IV thrombolysis, last-known-well-to-puncture time, and puncture to recanalization time.
4. Discussion
This retrospective cohort study provides insights into the outcomes of patients with AF and without AF who underwent EVT for anterior circulation occlusion at three comprehensive stroke centers in China. Our study showed no differences in early and long-term favorable outcomes between the two groups of patients.
Previous studies assessing complications related to EVT reported that AF was a significant risk factor for complications, especially intracranial hemorrhage. A retrospective analysis of consecutive patients presenting to 13 high-volume stroke centers revealed that AF compared to no-AF individuals with anterior circulation occlusion, had a significant risk of parenchymal hematomas [OR 1.61 (1.01–2.55), p < 0.045] (Nogueira et al., 2015). More recent cohort studies revealed that patients with AF and no-AF patients had better endovascular mechanical thrombectomy outcomes (90-day favorable outcome 55.8 vs. 17.5%, p < 0.01); however, this benefit was not persistent in elderly patients (>70 years) (Lin et al., 2020). In the present cohort, age did not affect the endovascular outcome in patients with or without AF.
We believe that the positive outcomes encountered in the present study can be attributed to two main factors. First, the development of the endovascular technique and devices probably influenced the outcomes. Second, the present cohort only included individuals with anterior circulation proximal LVO. In other studies, different territories were assessed, and a sub-analysis of their findings was later conducted.
A recent study by Zdraljevic et al. (2022) found that AF is an independent negative predictor of good long-term functional outcome (OR 0.29, 95% CI 0.11–0.78, p = 0.01). Therefore, there is a possible bias regarding the EVT procedure technique and selection bias. Moreover, another multicenter retrospective study assessing the clinical outcomes of 219 individuals with valvular versus non-valvular AF in acute anterior circulation occlusive stroke undergoing EVT showed that both groups had similar safety and functional outcomes (Li et al., 2019). The authors explained that chronic heart failure should be evaluated in stroke studies because this condition confers three times the risk of poor functional outcomes.
Furthermore, a Medicare study extracted data from 4,627 subjects who underwent EVT. In the unmatched cohorts, patients with AF were older and had a significantly greater burden of key comorbidities than the non-AF group (age 74 y ± 11 vs. 60 y ± 15, p < 0.0001) (Munir et al., 2017). However, there was no difference between the groups when mortality, morbidity, and even costs were evaluated (Munir et al., 2017).
Recently, a systematic review and meta-analysis including 10 studies with 6,543 patients conducted by Kobeissi et al. (2023) found that there were comparable rates of mRS scores of 0 to 2 between patients with AF and patients without AF (odds ratio [OR], 0.72 [95% CI, 0.47–1.10]; P = 0.13), with significant heterogeneity (I2 = 75%; P < 0.001) among the included studies. After sensitivity analysis, the rate of mRS scores of 0 to 2 was significantly lower among patients with AF (OR, 0.65 [95% CI, 0.52–0.81]; P < 0.001), with heterogeneity (I2 = 55%; P = 0.02). Noteworthy, there is significant heterogeneity among the included studies in Kobeissi et al.’s study. Heterogeneity was assessed using the Q statistic and the I2 test, in which I2 greater than 50% or P < 0.05 were considered significant. Therefore, we can conclude that further studies are required to examine the conclusion of Kobeissi et al. (2023). Additionally, the heterogeneity in the results may partially be attributed to the higher rates of diabetes and hypertension in the AF group in Kobeissi et al.’s study. An important factor that can modify the outcomes of patients undergoing EVT is the previous use of intravenous thrombolysis. Yaghi et al. (2020) assessed intravenous alteplase and its effects in AF patients with cardioembolic stroke. The authors revealed that thrombolysis could reduce the 90-day mortality of patients with acute ischemic stroke with AF not undergoing EVT (OR, 0.58; 95% CI, 0.39–0.87).
Other studies described age as an important risk factor for worse outcomes related to anterior circulation stroke after EVT (Castonguay et al., 2014; Lasek-Bal et al., 2022). However, in the HERMES meta-analysis, the subgroup of patients who were older still benefited significantly from EVT (Goyal et al., 2016). In this context, our study described the modeling as a determinant variable of 65 years, and favorable outcomes were encountered (Yousufuddin and Young, 2019). We believe that more studies regarding the definition of this variable as 65 years should be conducted to explain the influence of this independent variable better.
Globally, the population aged 65 and over is growing faster than all other age groups. Concurrently, there is a significant increase in cardiovascular risk factors and the development of atrial fibrillation. Therefore, studies assessing the influence of age on outcomes are essential for prognostic risk stratification. Moreover, studies of specific age groups of the population can lead to the development of new techniques and other practices promoting a favorable outcome.
Limitations of our study include the relatively small size of our sample. Secondly, our cohort was hospital-based and not population-based, which could have biased our results. Thirdly, the retrospective nature of this study may have resulted in information bias. Fourthly, we cannot exclude the introduction of bias caused by the different routines of each physician. Also, it is worth mentioning that no histopathological differentiation was done between red thrombi (red blood cell-rich) and white thrombi (fibrin-rich). Despite such limitations, the current study can highlight the significance of functional outcome after EVT in patients with AF who have anterior circular occlusion.
In conclusion, after adjusting for confounding factors such as age, male sex, chronic kidney disease, current smoking history, NIHSS Pre-EVT, mRS pre-treatment, IV thrombolysis, last-known-well-to-puncture time, and puncture to recanalization time, AF patients achieved similar outcomes as non-AF patients with anterior circulation occlusion treated with endovascular therapy.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The study was reviewed and approved by the Medical Ethical Committees of the Foshan Sanshui District People’s Hospital. Written informed consent from the participants’ legal guardians/next of kin was not required to participate in this study per the national legislation and institutional requirements. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author contributions
YC, WW, JP, HM, SY, and XL conceived the idea and drafted the manuscript. TN, MM, and DL provided critical revision. WL, WP, SZ, YL, JG, JW, ZO, and HW collected data and reviewed the manuscript. All authors contributed to the manuscript and read and approved the final version of the manuscript.
Funding
This study was supported by Foshan Science and Technology Bureau (Grant No. 2220001005022), Medical Science Technology Research Foundation of Guangdong Province (Grant No. 20221027164016611), the Foshan 14th Five-Year Plan Key Discipline Foundation, China, the Guangdong provincial TCM Bureau Key Discipline Foundation, China, and Foshan Competitive Talent Support Project Fund (Brain-Heart Talent Project-Build the Brain-Heart Comorbidity Multi-disciplinary Medical Center). Fund Project of Health Bureau of Foshan City of Guangdong Province in 2023 (Grant No. 20230309).
Acknowledgments
We would like to thank all colleagues for data collection and patient contribution.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Akbik, F., Alawieh, A., Dimisko, L., Howard, B. M., Cawley, C. M., Tong, F. C., et al. (2022). Bridging thrombolysis in atrial fibrillation stroke is associated with increased hemorrhagic complications without improved outcomes. J. Neurointerv. Surg. 14, 979–984. doi: 10.1136/neurintsurg-2021-017954
Arboix, A., Garcia-Eroles, L., Oliveres, M., Massons, J. B., and Targa, C. (1998). Clinical predictors of early embolic recurrence in presumed cardioembolic stroke. Cerebrovasc. Dis. 8, 345–353. doi: 10.1159/000015878
Castonguay, A. C., Zaidat, O. O., Novakovic, R., Nguyen, T. N., Taqi, M. A., Gupta, R., et al. (2014). Influence of age on clinical and revascularization outcomes in the North American Solitaire Stent-Retriever Acute Stroke Registry. Stroke 45, 3631–3636. doi: 10.1161/STROKEAHA.114.006487
Chen, Y., Zhou, S., Yang, S., Mofatteh, M., Hu, Y., Wei, H., et al. (2022). Developing and predicting of early mortality after endovascular thrombectomy in patients with acute ischemic stroke. Front. Neurosci. 16:1034472. doi: 10.3389/fnins.2022.1034472
Goyal, M., Menon, B. K., van Zwam, W. H., Dippel, D. W., Mitchell, P. J., Demchuk, A. M., et al. (2016). Endovascular thrombectomy after large-vessel ischaemic stroke: A meta-analysis of individual patient data from five randomised trials. Lancet 387, 1723–1731. doi: 10.1016/S0140-6736(16)00163-X
Jiao, J., Liu, S., Cui, C., Cao, Y., Jia, Z., Liu, H., et al. (2022). Endovascular thrombectomy for acute ischemic stroke in elderly patients with atrial fibrillation. BMC Neurol. 22:100. doi: 10.1186/s12883-022-02631-3
Junejo, R. T., Lip, G. Y. H., and Fisher, J. P. (2020). Cerebrovascular dysfunction in atrial fibrillation. Front. Physiol. 11:1066. doi: 10.3389/fphys.2020.01066
Kimura, K., Iguchi, Y., Shibazaki, K., Iwanaga, T., Yamashita, S., and Aoki, J. (2009). IV t-PA therapy in acute stroke patients with atrial fibrillation. J. Neurol. Sci. 276, 6–8. doi: 10.1016/j.jns.2008.10.018
Kobeissi, H., Ghozy, S., Seymour, T., Gupta, R., Bilgin, C., Kadirvel, R., et al. (2023). Outcomes of patients with atrial fibrillation following thrombectomy for stroke: A systematic review and meta-analysis. JAMA Netw. Open 6:e2249993.
Kornej, J., Borschel, C. S., Benjamin, E. J., and Schnabel, R. B. (2020). Epidemiology of atrial fibrillation in the 21st century: Novel methods and new insights. Circ. Res. 127, 4–20. doi: 10.1161/CIRCRESAHA.120.316340
Lasek-Bal, A., Zak, A., Binek, L., Student, S., Cieslik, A., Bal, W., et al. (2022). Relevance of admission hyperglycaemia and diabetes mellitus to efficacy and safety of mechanical thrombectomy in stroke patients. Neurol. Neurochir. Pol. 56, 472–479.
Li, W., Wang, S., Li, S., Chen, X., and Xiong, Y. (2019). Clinical outcomes of valvular versus nonvalvular atrial fibrillation in acute anterior circulation occlusive stroke undergoing endovascular treatment. J. Stroke Cerebrovasc. Dis. 28, 31–37. doi: 10.1016/j.jstrokecerebrovasdis.2018.09.009
Lin, C. J., Luo, C. B., Chien, C., Chang, F. C., Lin, C. J. I, Lee, H., et al. (2020). Better endovascular mechanical thrombectomy outcome in atrial fibrillation patients with acute ischemic stroke: A single-center experience. J. Chin. Med. Assoc. 83, 756–760.
Loo, J. H., Leow, A. S., Jing, M., Sia, C. H., Chan, B. P., Seet, R. C., et al. (2023). Impact of atrial fibrillation on the treatment effect of bridging thrombolysis in ischemic stroke patients undergoing endovascular thrombectomy: A multicenter international cohort study. J. Neurointerv. Surg. doi: 10.1136/jnis-2022-019590 [Epub ahead of print].
Munir, M. B., Alqahtani, F., Beltagy, A., Tarabishy, A., and Alkhouli, M. (2017). Comparative outcomes of mechanical thrombectomy for acute ischemic stroke in patients with and without atrial fibrillation. J. Vasc. Interv. Radiol. 28, 1604–1605.
Nogueira, R. G., Gupta, R., Jovin, T. G., Levy, E. I., Liebeskind, D. S., Zaidat, O. O., et al. (2015). Predictors and clinical relevance of hemorrhagic transformation after endovascular therapy for anterior circulation large vessel occlusion strokes: A multicenter retrospective analysis of 1122 patients. J. Neurointerv. Surg. 7, 16–21. doi: 10.1136/neurintsurg-2013-010743
Sanak, D., Herzig, R., Kral, M., Bartkova, A., Zapletalova, J., Hutyra, M., et al. (2010). Is atrial fibrillation associated with poor outcome after thrombolysis? J. Neurol. 257, 999–1003.
Turc, G., Bhogal, P., Fischer, U., Khatri, P., Lobotesis, K., Mazighi, M., et al. (2019). European Stroke Organisation (ESO)- European Society for Minimally Invasive Neurological Therapy (ESMINT) guidelines on mechanical thrombectomy in acute ischemic stroke. J. Neurointerv. Surg. 11, 535–538.
Yaghi, S., Mistry, E., Liberman, A. L., Giles, J., Asad, S. D., Liu, A., et al. (2020). Anticoagulation type and early recurrence in cardioembolic stroke: The IAC study. Stroke 51, 2724–2732. doi: 10.1161/STROKEAHA.120.028867
Yang, S., Yao, W., Siegler, J. E., Mofatteh, M., Wellington, J., Wu, J., et al. (2022). Shortening door-to-puncture time and improving patient outcome with workflow optimization in patients with acute ischemic stroke associated with large vessel occlusion. BMC Emerg. Med. 22:136. doi: 10.1186/s12873-022-00692-8
Zdraljevic, M., Pekmezovic, T., Stanarcevic, P., Vukasinovic, I., Berisavac, I., Ercegovac, M., et al. (2022). Atrial fibrillation is associated with poor long-term outcome after mechanical thrombectomy for anterior large vessel occlusion stroke. J. Stroke Cerebrovasc. Dis. 31:106755. doi: 10.1016/j.jstrokecerebrovasdis.2022.106755
Keywords: cerebrovascular, atrial fibrillation, stroke, endovascular thrombectomy (EVT), patient outcome, occlusion
Citation: Wu W, Pitton Rissardo J, Nguyen TN, Mofatteh M, Wei H, Liebeskind DS, Yang S, Li W, Pan W, Zhou S, Lai Y, Gao J, Wang J, Ouyang Z, Mai Y, Meng H, Chen Y and Liao X (2023) Effect of atrial fibrillation on outcomes in patients with anterior circulation occlusion stroke receiving endovascular therapy. Front. Aging Neurosci. 15:1160265. doi: 10.3389/fnagi.2023.1160265
Received: 07 February 2023; Accepted: 30 May 2023;
Published: 15 June 2023.
Edited by:
Marialuisa Zedde, IRCCS Local Health Authority of Reggio Emilia, ItalyReviewed by:
Adria Arboix, Sacred Heart University Hospital, SpainAntonio Arjona, Independent Researcher, Almería, Spain
Copyright © 2023 Wu, Pitton Rissardo, Nguyen, Mofatteh, Wei, Liebeskind, Yang, Li, Pan, Zhou, Lai, Gao, Wang, Ouyang, Mai, Meng, Chen and Liao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yimin Chen, drymchen@126.com; Heng Meng, memphisheng@163.com; Xuxing Liao, drliao210409@163.com
 Weijuan Wu1
Weijuan Wu1  Jamir Pitton Rissardo
Jamir Pitton Rissardo Thanh N. Nguyen
Thanh N. Nguyen Mohammad Mofatteh
Mohammad Mofatteh David S. Liebeskind
David S. Liebeskind Ziqi Ouyang
Ziqi Ouyang Yimin Chen
Yimin Chen Xuxing Liao
Xuxing Liao